Several Blue Cross Blue Shield health plans across the country reported net losses in 2024, raising concerns about the financial stability of some of the nation’s largest nonprofit insurers.
Independence Health Group, the for-profit parent company of the nonprofit Philadelphia-based Independence Blue Cross, posted a net loss of $239 million, despite generating $32 billion in revenue. The company cited a sharp rise in medical and pharmacy costs as the main factor behind the losses.
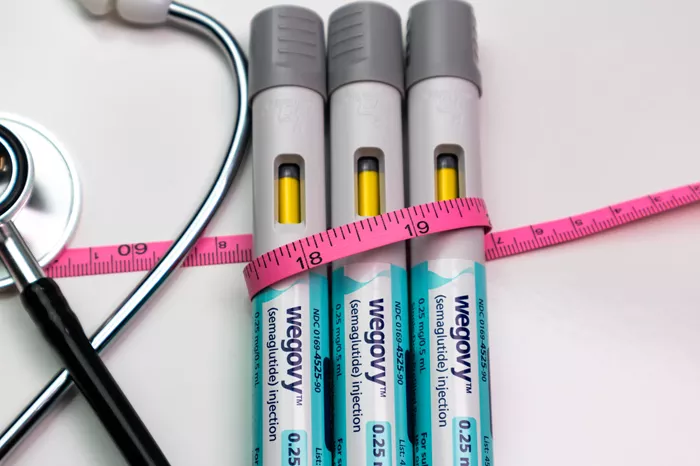
A significant contributor to these losses is the rapid growth in weight-loss medications, particularly glucagon-like peptide-1 receptor agonists (GLP-1s), such as Ozempic, which help manage blood sugar levels. In 2023, Independence Health Group spent $350 million on GLP-1 medications for its members, a figure that soared to $500 million in 2024.
The company, which operates in 32 states and Washington D.C., also experienced reduced profitability in its Medicaid and Medicare programs. The cost of care in these programs outpaced rate increases, and the number of Medicaid recipients requiring care was higher than expected.
Changes to Medicaid coverage, which had been continuously extended during the COVID-19 pandemic, also contributed to financial pressures. In 2023, states began re-evaluating Medicaid eligibility annually, leading to uncertainty about the health needs of enrollees.
Elizabeth Williams, a senior policy manager for Medicaid research at the Kaiser Family Foundation, explained that both states and health plans struggled to predict the health needs of Medicaid recipients who remained on the program. This resulted in higher-than-expected health costs.
In Pennsylvania, one of 13 states that approve GLP-1 medications for the treatment of obesity, Medicaid patients also contributed to the surge in demand for these drugs.
Nationwide, the number of GLP-1 prescriptions skyrocketed by 400% between 2019 and 2023, according to a Kaiser Family Foundation survey. Medicaid’s total spending on these medications reached $3.9 billion in 2023, up from $1.9 billion in 2022. These medications can cost up to $1,000 per month per person.
Insurance companies typically set their premiums a year in advance, meaning they cannot adjust rates mid-year. If they face unexpected costs, like those from weight-loss drugs, they must recover the losses in the following year by raising premiums.
The Affordable Care Act mandates that health insurers spend at least 80% of premiums on health care costs and quality improvements, with the remainder going toward overhead costs. This means that insurers must raise prices in the next cycle to compensate for losses, hoping that customers will stay with the plan.
Ben Handel, an economics professor at the University of California, Berkeley, explained that the high demand for GLP-1 medications, coupled with their steep cost, has led to a significant rise in insurance claims. Around 42% of adults under 65 with private insurance could be eligible for these weight-loss drugs, according to the U.S. Food and Drug Administration.
“The challenges we faced at Independence Health Group were felt throughout the health care industry, impacting both Blue Cross Blue Shield plans and publicly traded insurers,” said Juan Lopez, executive vice president and CFO of Independence Health Group.